- Pharmaceutical Technology-04-01-2009
- Volume 2009 Supplement
- Issue 1
Influence of Superdisintegrants on the Rate of Drug Dissolution from Oral Solid Dosage Forms
The authors examine common superdisintegrants (i.e., crospovidone Type A, crospovidone Type B, croscarmellose sodium, and sodium starch glycolate) with a set of poorly soluble drug actives and evaluate in vitro drug dissolution.
Dissolution is essential for a drug to be absorbed through the biological membranes into systemic circulation for therapeutic efficacy. Conventional tablet formulations generally require rapid disintegration to aid drug dissolution. Superdisintegrants are added to oral solid dosage formulations to facilitate disintegration. Commonly used superdisintegrants such as crospovidone, croscarmellose sodium, and sodium starch glycolate are highly efficient at low concentration levels (2–5 w/w%) in the tablet formulation at facilitating the rate and extent of tablet disintegration. The correlation between tablet disintegration and drug dissolution, however, is not always observable (1–3).
Table I
One recent study, for example, evaluated the respective effects of crospovidone, croscarmellose sodium, and sodium starch glycolate on the dissolution behavior of eight cationic drugs from a model direct-compression tablet formulation with 2% w/w superdisintegrant (4). No significant differences were observed in the disintegration times of the tablets. However, the study did show that crospovidone demonstrated a more rapid dissolution rate than the other superdisintegrants for the cationic drugs studied, irrespective of the drug's aqueous solubility.
Table II
The dissolution studies were performed for each drug in the compendial media for the drug. Crospovidone provided the fastest dissolution in the compendial media for seven of the eight drugs. Because crospovidone is nonionic, ionic interaction between this superdisintegrant and the cationic drug was impossible. In contrast, croscarmellose sodium and sodium starch glycolate are both anionic, and these superdisintegrants could potentially interact with cationic drug actives and slow their dissolution. As a result of these observations, the authors recommended formulation screening of superdisintegrants during excipient selection to minimize dissolution retardation resulting from any drug–excipient interaction.
Table III
More than 60% of new drugs currently in development today are considered poorly soluble, as are nearly half of the drugs whose patents will expire in the next 10 years. Selecting formulation ingredients that enhance the dissolution of poorly soluble drugs has therefore become increasingly important to achieve therapeutic efficacy. Once a tablet disintegrates, the solubility properties of the drug, either alone or assisted by other formulation ingredients, determine the drug's subsequent dissolution rate and extent of release. Water-soluble drugs provide rapid and high-level drug release. However, other ingredients in the formulation of poorly soluble drugs, including the disintegrant, must play a key role in determining the finished formulation's drug-dissolution characteristics. With that in mind, this study was conducted to explore the impact of superdisintegrant selection on the rate of dissolution of poorly soluble drugs.
Table IV
Experimental materials and methods
Materials. Table I lists the 13 poorly soluble active ingredients tested. Their aqueous solubilities were 2–2300 µg/mL. The superdisintegrants studied were crospovidone Type A (Polyplasdone XL, International Specialty Products, ISP, Wayne, NJ), crospovidone Type B (Polyplasdone XL-10, ISP), croscarmellose sodium (Ac-Di-Sol, FMC Biopolymer, Philadelphia, PA), and sodium starch glycolate (Glycolys, Roquette, Tokyo). As outlined in the European Pharmacopoeia, crospovidone is available in different particle sizes. Crospovidone Type B has a smaller average particle size than crospovidone Type A.
Table V
Tablet preparation. Tablets were prepared at the highest market dose using a direct compression (DC) or wet granulation (WG) process as considered appropriate through a review of the ingredients listed in the Physician's Desk Reference (PDR) and patent literature.
Table VI
For tablets prepared by direct compression, required ingredient quantities were weighed and blended to form a homogeneous powder mix. The blends were then compressed using appropriate tooling on a 16-station, instrumented, rotary compression machine (CMD4, Cadmach, Ahmdedabad, Gujarat, India). Advanced Instrumentation Monitor (AIM) software, (Metropolitan Computing Corporation, East Hanover, NJ) was used with the tablet press to determine the compression force required to yield tablets of approximately equal hardness for the various drugs used in the study. Formulations used to prepare atorvastatin and loratadine tablets by direct compression are shown as examples in Tables II and III, respectively.
Table VII
For tablets prepared by wet granulation, weighed amounts of drug, diluent, and binder were premixed for 60 s in a granulator bowl (4M8, Pro-C-Ept, Zelzate, Belgium) at an impeller speed ranging from 1000 to 1200 rpm. Water was added at a predetermined rate, and after 120 s, the chopper was started (2300–2500 rpm). Granulation proceeded for 10 min. The impeller torque and the product temperature were monitored to determine the end point of granulation. The granules were sieved through specified mesh and dried in an oven at 60 °C, to a final moisture content of 1.5–2% w/w, measured using a moisture balance (MA45, Sartorius, Goettingen, Germany). The required quantities of remaining ingredients were weighed and blended with the granules to form a homogeneous powder mix. The blends were then compressed as previously described. Formulations used to prepare efavirenz and ezetimibe tablets by wet granulation are shown as examples in Tables IV and V, respectively.
Table VIII
Tablet evaluation .Tablet strength. The respective breaking forces of the prepared tablets were determined 24 h after compression using a hardness tester (TBH 310 MD, ERWEKA, Heusenstamm, Germany). Ten tablets from each batch prepared were tested for tablet breaking force, and the mean and standard deviation were calculated.
Table IX
Disintegration time. Respective disintegration times of the prepared tablets were measured in 900 mL of purified water with disks at 37 °C using a TAR series tester (ERWEKA). Disintegration times of six individual tablets were recorded.
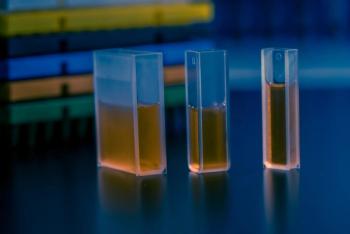
Figure 1 (All figures are courtesy of the authors)
In vitro dissolution. The dissolution studies of the prepared tablets were carried out using US Pharmacopeia (USP) Apparatus 2 (Vankel VK, Palo Alto, CA). Dissolution profiling was performed with the medium recommended by USP or the US Food and Drug Administration for the respective drug. Dissolution profiling was also carried out in a medium developed in house and derived from the recommended media, capable of discriminating between the formulations. A peristaltic pump was coupled to a UV–visible spectrophotometer (Carry 50, Palo Alto, CA) to provide a continuous flow of the drug solution through a 1-cm cuvette. Samples were programmed to be analyzed at 5, 10, 15, 30, 45, and 60 min at the λ max of the respective drugs. The time required to achieve 80% drug release (t80) was considered for comparing dissolution results. The t80 was determined by fitting the dissolution data to a four-parametric logistic model using the Marquardt–Levenberg algorithm (Sigmaplot 9.0, SPSS, Chicago).
In this equation, y represents the cumulative percent of drug released, x is the time in minutes, "min" is the baseline of percent drug released at 0 min, "max" is the plateau of percent drug released at 60 min, and "hillslope" is the slope of the curve at transition center EC50.
Figure 2
Results and discussion
Although crospovidone, croscarmellose sodium, and sodium starch glycolate are used to provide the same function within the formulation, they differ in their chemical structure, particle morphology, and powder properties.
Figure 3
Croscarmellose sodium is the sodium salt of a cross-linked, partly O-(carboxymethylated) cellulose, and sodium starch glycolate is the sodium salt of a carboxymethyl ether of starch or of a cross-linked carboxymethyl ether of starch (5). Both materials are sodium salts and are anionic. In addition, their polymer backbones are composed mostly of glucose repeat units. In contrast, crospovidone is an insoluble, cross-linked homopolymer of N-vinyl-2-pyrrolidone and is nonionic. Chemically, the repeat structure of crospovidone is similar to that of N-methylpyrrolidone, a water-miscible, polar aprotic solvent with high interfacial activity used as a solubilizer in many applications.
Figure 4
When examined under a scanning electron microscope, croscarmellose sodium particles have a fibrous, nonporous structure; sodium starch glycolate particles are spherical and nonporous; and crospovidone particles (Type A and Type B) appear highly porous and granular (see Figures 1–4). Both crospovidone types have similar particle morphology, but differ in particle size. Table VI shows a comparison of the superdisintegrants' typical average particle size and surface area (Mastersizer, Malvern, Worcestershire, England) and Brunauer, Emmett, and Teller gas adsorption, respectively. Crospovidone Type B had the smallest particle size and the highest surface area. The high surface area increases interfacial activity that can aid in drug dissolution. Thus, the unique chemical structure and powder properties of crospovidone Type B may improve the dissolution of poorly soluble drugs.
Figure 5
Drug-dissolution profiles are increasingly used to evaluate drug-release characteristics of pharmaceutical products. The dissolution media adopted by the pharmacopeias or recommended by FDA for in vitro dissolution testing are designed to maximize drug release. Thus, the recommended medium for a given marketed drug becomes the quality-control standard to ensure that batch-to-batch consistency and continuing product quality and performance are maintained regardless of changes in the manufacturing process. Although the recommended media for in vitro dissolution testing can guide formulation development, it typically does not discriminate between formulation ingredients because a poorly soluble drug's release is usually affected more by the medium than the formulation ingredients.
Figure 6
Discriminatory dissolution profiles are highly desirable for distinguishing between products with different pharmaceutical attributes (e.g., formulation or manufacturing-process differences) (6). In the present study, dissolution testing was conducted in the recommended media for the drug as well as in modified dissolution media that were designed to produce drug-release profiles that discriminate between formulations with different superdisintegrants. The formulations for a given drug were produced using the same process, ingredients, and ingredient levels. In addition, tablets were compressed to equivalent hardness to minimize the effect of the tablet's physical properties on the dissolution results. Only the selection of superdisintegrant varied. The discriminating media were selected so that at least one formulation achieved 80% drug release. Table VII shows the recommended and discriminating media for each drug tested.
Figure 7
For the 13 poorly soluble drugs evaluated, no significant differences were observed in the breaking force and disintegration times of the tablets prepared using the various superdisintegrants for a given drug studied (see Table VIII).
Figure 8
Figures 5–12 show the dissolution profiles for the tablets with atorvastatin, loratadine, efavirenz, and ezetimibe in the recommended and discriminating media as examples. The dissolution profiles indicate that the tablets with crospovidone Type B, in both the recommended and discriminating media, had the fastest rate of dissolution. Thus, even though the superdisintegrants gave similar disintegration results, the choice of superdisintegrant had a significant effect on drug dissolution. Because the discriminating media showed even greater differences in dissolution rate between the superdisintegrants studied, the discriminating media were highly effective at identifying differences between the superdisintegrants selected.
Figure 9
Table IX shows the t80 results for all 13 drugs studied in both media. In the recommended media, crospovidone provided the fastest t80 for 12 of the 13 drugs studied. Crospovidone Type B provided the fastest t80 for 10 of the 13 drugs studied. In the discriminating media, crospovidone Type B provided the fastest release for all drugs. A discriminating medium for raloxifene HCl tablets was not developed because the recommended medium was sufficiently discriminating. Therefore only 12 drugs were evaluated in a discriminatory medium. Furthermore, crospovidone Type B was often the only superdisintegrant to yield a formulation of the most poorly soluble drugs that achieved 80% drug release in the discriminating media. Overall, the results suggest that crospovidone Type B is more effective than the other superdisintegrants in enhancing the dissolution rate of poorly soluble drugs. Crospovidone Type B has solventlike chemistry and high surface area, resulting in high interfacial activity that enhances drug dissolution and release.
Figure 10
Conclusion
At a time when formulators are faced with increasing numbers of poorly soluble drugs, it has become very important to select superdisintegrants to maximize drug dissolution. A comprehensive study conducted to evaluate the effect of crospovidone, croscarmellose sodium, and sodium starch glycolate on the dissolution rates of poorly soluble drugs with varying aqueous solubility showed crospovidone Type B to provide the fastest rate of dissolution for poorly soluble drugs. The fact that tablet strength and disintegration times for the tablets containing each drug and all the superdisintegrant studies were similar showed that tablet hardness and disintegration did not influence dissolution. Crospovidone Type B has unique chemistry, particle size, and particle morphology that result in high interfacial activity, which significantly aids dissolution.
Figure 11
Acknowledgments
The authors wish to acknowledge the support and contributions of ISP's pharmaceutical research and development and analytical scientists in Hyderabad, India, and Wayne, New Jersey.
Figure 12
Jagdish Balasubramaniam is a manager of pharmaceutical research and development at International Specialty Products India, and Tim Bee* is a senior director of pharmaceuticals at International Specialty Products, 1361 Alps Rd., Wayne, NJ 07470, tel. 973.628.4148,
*To whom all correspondence should be addressed.
References
1. J.R. Johnson et al., "Effect of Formulation Solubility and Hygroscopicity on Disintegrant Efficiency in Tablets Prepared by Wet Granulation, in Terms of Dissolution," J. Pharm. Sci. 80 (5), 469–471 (1991).
2. J.K. Pandit, M.K. Tripathi, and R.J. Babu, "Effect of Tablet Disintegrants on the Dissolution Stability of Nalidixic Acid Tablets," Pharmazie 52 (7), 538–540 (1997).
3. A. Sakr, M. Bose, and A. Menon, "Comparative Effectiveness of Superdisintegrants on the Characteristics of Directly Compressed Triamterene Hydrochlorothiazide Tablets," Pharm. Ind. 55 (10), 953–957 (1993).
4. J. Balasubramaniam et al., "Effect of Superdisintegrants on Dissolution of Cationic Drugs," Dissolution Technologies 15 (2), 18–25 (2008).
5. USP 31–NF 26 (US Pharmacopeial Convention, Rockville, MD, 2008).
6. S.A. Qureshi, "Developing Discriminatory Drug Dissolution Tests and Profiles: Some Thoughts for Consideration on the Concept and Its Interperatation," Dissolution Technologies 13 (4), 18–23 (2006).
Articles in this issue
almost 17 years ago
Using Polymers to Enhance Solubility of Poorly Soluble Drugsalmost 17 years ago
A Novel Pregelatinized Starch as a Sustained-Release Matrix ExcipientNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.