- Pharmaceutical Technology-06-02-2017
- Volume 41
- Issue 6
Understanding Dissolution Testing
Industry experts discuss best practices for dissolution testing of poorly soluble, immediate-release, and controlled-release formulations and the different analytical approaches used.
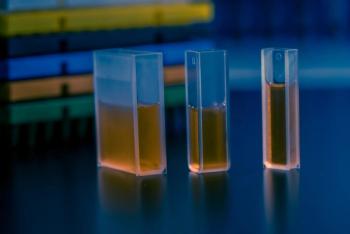
Dissolution testing provides crucial in-vitro drug release information that is routinely used for quality-control (QC) and quality-assurance (QA) purposes in the pharmaceutical industry. The quality-by-design (QbD) approach places strong emphasis on the role of dissolution testing in optimization of a formulation’s drug release rate and evaluation of critical process parameters (CPPs) in the manufacturing process that may affect performance of the dosage form, notes Bryan Crist, scientific affairs manager, Agilent Technologies. “Data from dissolution studies form an essential component in regulatory submissions and all stages of the approval process,” he says. “Post approval, the dissolution test provides continual assurance of batch-to-batch consistency in product performance as well as the ability to reject sub-performing batches. Additionally, scale-up and post-approval changes (SUPAC) guidance relies heavily on dissolution testing to assure that these routine post-approval activities do not impact product performance.”
According to Marcel Arndt, head of Dissolution Laboratory, Evonik Health Care, a QC dissolution test should be discriminative for critical quality attributes (CQA) of a pharmaceutical product. The dissolution rate can significantly affect bioavailability, he highlights; therefore, the dissolution test and acceptance criteria should distinguish batches with unacceptable bioavailability. “Risk assessments and definition of quality target product profiles are used throughout development and lifecycle management to identify potentially high-risk formulation and process variables. Design of experiment (DOE) procedures, which include dissolution testing, can be used to achieve an improved product and process understanding to develop an appropriate control strategy. A design space can then be defined based on dissolution test results,” he explains.
During product lifecycle management, the dosage form or formulation constitution might change, Andreas Gryczke, global technical marketing manager, Solubilization at BASF, points out. In such cases, it is important that the dissolution test is reviewed critically.
Pharmaceutical Technology spoke with Bryan Crist, Andreas Gryczke, and Marcel Arndt about best practices for dissolution testing of poorly soluble, immediate-release, and controlled-release formulations and about the different analytical approaches used.
Challenges in dissolution testing
PharmTech: What are the challenges in dissolution testing?
Gryczke (BASF): Dissolution testing is still a model with constraints. The main challenge lies in establishing a proper in vitro-in vivo correlation due to differences between human beings--for example, pH, drug residence time in the gastrointestinal (GI) tract, and the viscosity caused by food consistency can vary from individual to individual, influencing the drug release and ultimately drug absorption.
Arndt (Evonik): For QC purposes, the challenge is to design a dissolution test method that can distinguish between different product qualities as a surrogate for predicting acceptable or nonacceptable bioavailability. For development purposes, the challenge is to achieve a dissolution test method that is able to sufficiently simulate the GI physiology in order to predict how the formulation will behave in vivo (e.g., for de-risking clinical studies).
There are also several technical challenges to overcome. Just to mention a few: Coning is an issue in dissolution tests, where undissolved material forms a mound in the stagnant zone below the paddle, which inhibits dissolution and can be overcome by either adapting the stirring speed or by using peak vessels. Capsules may require the use of a sinker (a stainless-steel wire helix) to prevent the dosage form from floating to the surface of the dissolution media, which would otherwise result in variable dissolution. Filter clogging can restrain online ultraviolet (UV) measurements or block systems using the United States Pharmacopeia (USP) IV test setup. Undissolved particles forming a turbid suspension limit the use of fiber optic UV dissolution systems. Additionally, conducting dissolution tests for lipid formulations, which are often filled in soft gelatin capsules, can result in the floating of the low-density lipid matrix and prevent adequate mixing in the USP I and II dissolution test setups.
Crist (Agilent): Manual dissolution testing can introduce technique-dependent variability into the test and for this reason, automation is often sought as a way to standardize the dissolution with less analyst-to-analyst variability. The five major areas of the dissolution test are typically: setup, executing the test, sampling, sample analysis, and cleaning. Testing, whether manual or automated, still relies heavily upon the analyst’s level of training and attention to detail contained in dissolution standard operating procedures (SOP) and analytical procedures.
Setup challenges begin with media preparation, which must be exactly as dictated in the dissolution method, including deaeration if required. Observational checks must ensure that the apparatus is clean, in proper condition, properly adjusted, and that sources of environmental vibration are absent from the area. Manual or automated sampling equipment must be clean and ready for use with the proper disposable filters.
Challenges for executing the test begin with the media being accurately measured and introduced into the vessels to control the volume within 1% of its total volume through the test period with proper evaporation covers. The timing begins with samples introduced into non-rotating media; the samples must settle to the bottom prior to rotation. Dosage units should be observed to confirm they are present and not floating.
The main sampling challenge involves introducing dosages simultaneously because samples must be withdrawn within 2% of the time they were dropped. For a 30-minute sample, this means you have ± 36 seconds to pull all six samples at the correct midway position and filter all of them into their respective vials or tubes; this is one of the primary reasons the dissolution test may be automated.
Analytical procedures (whether using UV or high-performance liquid chromatography [HPLC]) have their own set of challenges, and the testing concludes by performing a validated cleaning procedure to ensure that all traces of the product and media are removed from the dissolution equipment.
Approaches and techniques
PharmTech: What are the different approaches and techniques used in dissolution testing? What are the pros and cons of the different approaches and techniques?
Arndt (Evonik): The basket (Type I) and paddle (Type II) USP apparatus are by far the most widely used dissolution test equipment. Both are extensively recommended in the individual USP monographs as QC methods. The basket and paddle apparatus can cover a wide range of oral dosage forms, with the basket apparatus having particular advantages in the testing of multiparticulate dosage forms. A limitation of both the USP I and USP II apparatus is the inability to use volumes other than in the 500-1000 mL range, which thereby restricts the use of biorelevant volumes under certain GI conditions (e.g., fasted state gastric volume) in contrast to the USP IV flow-through cell apparatus.
When detailed GI transit with multiple test media is required, for example, for pH-sensitive modified-release dosage forms, the USP III reciprocating cylinder is far more appropriate than either the basket or paddle apparatus. Another advantage of the USP III apparatus is that the more disintegration tester like hydrodynamics, keep lipid formulations dispersed in the dissolution media, which may float without any mixing in a USP I or II setup. However, because the operating volume for each vessel of the reciprocating cylinder is comparably low, it may be difficult to generate sink conditions, which may be a crucial factor especially for poorly soluble drugs.
The USP IV apparatus is described mainly for oral modified-release dosage forms testing, but can also be used for suppositories, parenteral depot dosage forms, suspension-type extended-release dosage forms, or microparticles. For this apparatus, however, certain variables including the size of the glass beads and filter material used to maintain the formulation in the sample cell may influence the hydrodynamic behavior, thereby, making it difficult to interpret the dissolution profile. A detailed review of the different dissolution equipment is given by Kostewicz et al. (1).
Crist (Agilent): Dissolution and drug release apparatus are quite flexible to accommodate numerous dosage forms, and the requirements for testing have continued to evolve well beyond traditional oral medicines requiring only the paddle or basket apparatus. Due to alternative routes of drug administration and delivery modifications, special apparatus have been developed over the years to address products ranging from topical forms (e.g., transdermal systems, ointments, creams, and gels) to implants (e.g., drug eluting stents, pacemaker leads, and mesh); as well as injectable dosage forms incorporating micro- and nanomedicines.
Many of these injectables or implants rely on targeted drug delivery that contain very small quantities of API. To address these needs, typical apparatus have been miniaturized to allow dissolution in small-volume vessels in 50-200 mL or less, with reciprocating holder apparatus now capable of precise and accurate drug release testing in only 5 mL. In contrast, veterinary bolus dosage forms containing grams of active drug may require 2 L or even larger-volume systems to accommodate sink conditions required to solubilize the drug during the dissolution test.
These alternatives have provided essential product performance testing platforms to the pharmaceutical industry usually through joint collaborations with drug product and dissolution apparatus development teams. Because many of these apparatus modifications are made for new and proprietary drugs, however, the knowledge of these alternative methods of analysis unfortunately remains non-available to the public even though the new apparatus platforms are commercially available.
Gryczke (BASF): Nowadays, many different dissolution test models exist. Some models such as the USP standard methods are well established, while others are complex because they try to replicate in detail in-vivo GI conditions, including the aspect of drug absorption. For QC of controlled- and immediate-release dosage forms, methods such as the USP Dissolution Apparatus 1 and 2 are suitable; whereas methods such as the reciprocating cylinder and the flow-through cell are suitable to reflect the requirements of the major challenges in achieving a sufficient bioavailability, such as in poorly soluble API formulations using polymers as a solubilizer.
At BASF, we collaborate closely with academia (e.g., University of Copenhagen) to implement more sophisticated dissolution test models for poorly soluble drugs. An example is the so-called acceptor-donor-model that includes the aspect of biphasic dissolution, which we use for both polymer-based amorphous solid dispersions and triglyceride-based self-emulsifying drug-delivery systems.
New approaches such as Permeapad, a multiwell plate system from the University Odense, Denmark, help to study the aspect of drug absorption better. For soft-gelatin capsule formulations, we use the same dissolution test model as for amorphous solid dispersions, but with the addition of a lipolysis model. For dermatologic formulations, the ‘Franz Cell’ apparatus is a suitable method.
Beside the apparatus, the media play an important role. In our lab, for example, we have moved away from using simple buffer and hydrochloric acid and now use biorelevant media containing sodium taurocholate, lecithin, and pepsin, which mimic a fasted state or fed state. Lastly, the aspect of enzymatic degradation can be reflected by using a pancreatin-based lipolysis model if the formulation requires this aspect. These complex test media provide the advantage of measuring dissolution in a more biorelevant environment. Using the in-vitro and in-vivo data together with the available performant statistical test methods allow us to build complex and precise computer models that can more accurately predict the drug release performance of a dosage form.
Analytical practices
PharmTech: What would you describe as acceptable analytical practices for dissolution testing of poorly soluble, immediate-release, and controlled-release formulations?
Crist (Agilent): Most solid oral-dosage forms fall into the categories of immediate release and some form of controlled release--extended, modified, or sustained. Immediate-release products are formulated to dissolve the API(s) within 30 minutes, at which time a single time point requiring at least 80%, typically, of the label claim to be in solution is demonstrated. Immediate-release drugs that are designed to release up to an hour will require a second time point to verify a release profile through that period.
Controlled-release testing requirements may vary greatly due to the wide variety of dosage forms that fall into this category. Most require drug release profiles consist of at least three time points: initial, midpoint, and final. The initial point early in the dosing period ensures that there is no dose dumping (i.e., a sudden and uncontrolled release of the drug). The midpoint determination ensures that the profile is controlling the release as expected about halfway through the release period, by concentration with most extended-release products, or by time with most sustained-release products. The final time point, usually near the end of the dosing interval, serves to indicate that typically a minimum of 80% of the drug is in solution and is available for absorption.
Drug solubility plays heavily into the suitability of the drug product formulation to fully release the active component(s) when expected, whether it is an immediate- or controlled-release product. Poor API solubility can be improved by providing salt or amorphous forms to increase its rate. Many poorly soluble drugs, however, require additional dissolution practices to solubilize the drug product, including the addition of surfactants or increased agitation. Higher volumes of dissolution media are occasionally required and used in special 2-L dissolution apparatus that are available for these purposes.
Gryczke (BASF): In immediate-release formulations, such as pellets of bitter tasting drugs coated with a polymer for taste-masking and moisture protection (e.g., Kollicoat Smartseal), the polymer dissolution is pH dependent. Therefore, it is necessary to establish a realistic pH-over-time profile.
The challenge of controlled-release formulations containing freely soluble APIs and based on sustained-release polymers is to guarantee that under all circumstances (e.g., low and high alcohol concentrations, fasted and fed state), the dissolution release profile is constant. In this case, the dissolution test needs to reflect not only on media constitution, such as ethanol concentration and bile salt concentration, but also on hydrodynamic influencing parameters, such as paddle speed.
For poorly soluble APIs, the two core aspects of formulation are:
- To bring the API into the saturated solution (e.g., by using vinylpyrrolidone-vinyl acetate copolymers in amorphous solid dispersions)
- To maintain the API in a supersaturated state until it is absorbed (e.g., by using solubilizers).
The challenge for poorly soluble materials is to generate a suitable calibration curve. Because this curve cannot be developed in water, typically an organic solvent-based HPLC method is used to determine the correct API concentration in different resulting phases--for example, aqueous phase, lipid phase if adequate, and pellet phase for crystallites. In summary, we can say that one needs to specify first what the critical parameters for the dissolution test are and then develop the corresponding method.
Arndt (Evonik): For development projects with poorly soluble drugs, biorelevant media such as Fasted (FaSSIF) or Fed State Simulated Intestinal Fluid (FeSSIF) should be considered. These media contain solubilizing ingredients such as bile salts and phospholipids at physiological concentrations, and therefore, are more precise in simulating the in-vivo solubility and dissolution rate of poorly soluble compounds than pure buffer media. Also, dissolution volumes used in the in-vitro test can be adapted to better reflect the physiological situation. Dissolution testing for QC purposes may require a non-physiological pH or the addition of solubilizers, such as sodium lauryl sulfate, to enable different product qualities to be differentiated based on the dissolution behavior.
For dissolution testing of standard immediate-release formulations using either the USP apparatus I or II, the test setup is in general less complex and of shorter duration compared to the test setup for controlled release dosage forms. According to the European Pharmacopoeia (Ph.Eur.), one suitable dissolution medium needs to be used for conventional release solid-dosage forms. In contrast, a two-stage test is required for delayed release dosage forms. An acid stage of 2 hours, in which the formulation should release less than 10%, is followed by a buffer stage at pH 6.8, in which rapid release is targeted. Controlled-release formulations, which target a release in the colon, could even require another buffer stage at pH 7.2, for example. Dissolution testing with increased change of media can be more convenient using USP III apparatus. However, there are also controlled-release dosage forms for which the release rates are robust to variations in GI physiology (e.g., many osmotic pump formulations aim for a prolonged release at zero-order, and therefore, do not require a change of dissolution medium).
PharmTech: Can you outline how to develop and validate a discriminating in-vitro dissolution test?
Arndt (Evonik): A dissolution test procedure intended to be used as a routine control test for drug products should be robust, reproducible, and discriminatory to ensure consistent product quality. The formulation prototype should, therefore, be tested during development under various conditions in-vitro (e.g., media, pH, apparatus, agitation) to identify a suitable method. Preliminary tests, such as API solubility and stability in the respective media, and filter compatibility studies can contribute to the test setup. Testing conditions, including sampling time points and frequency, should be chosen to provide the most suitable discrimination. If a surfactant is used in the dissolution media, the amount needed should be justified. After the identification of an appropriate QC dissolution test which is discriminative for CQAs of the drug product, the validation process can be initiated; it should include the following parameters.
The validation of the dissolution method should involve specificity testing to ensure that there is no interference with other components (e.g., excipients or dissolution media ingredients). Also, accuracy as well as linearity over the calibration range need to be examined and should cover the lowest expected concentration to more than the highest concentration during release testing. Precision testing (by performing replicate measurements of standard solutions) and intermediate precision/ruggedness testing (e.g., by repeating a run by at least two different analysts and different equipment from the same laboratory) also need to be performed as well as stability testing of standards and sample solutions. In later development phases, robustness should be part of the validation as well, which involves deploying deliberate changes to the dissolution conditions to determine an analytical design space.
Crist (Agilent): The complexity of developing a discriminating dissolution test is highest with new innovative products and novel delivery systems that have little or no public information. It is less complex for generic-drug products, for which there may be an abundance of public information available.
Development requires information including solubility determinations, intrinsic dissolution, sink condition (which will assist with volume considerations), and selection of the intended biorelevant media similar to fluid at in-vivo sites where dissolution occurs. This information will ultimately help with apparatus selection and the required agitation to provide a discriminating dissolution profile.
Sample filtration ensures that the integrity of the sample obtained during the test is preserved by removing undissolved drug substance and clarifying the sample without binding drug substance for analytical measurement. Additional method development tasks include setting specifications of specific dissolution time points, defining analytical methods of analysis, identifying the need to use sinkers, and justification for alternative test methods or components other than established harmonized pharmacopeial dissolution and drug release procedures.
When the crucial steps have been developed and a method is written, it must be validated to ensure it is accurate and precise and as robust as possible. Validation steps should challenge media preparation and deaeration, filters and cleaning procedures, analytical solution stability, and calculations accounting for analyte and volume loss. The analytical method must demonstrate linearity, range, specificity, accuracy, recovery, and precision. It is crucial that the suitably developed dissolution method will ultimately discriminate between a good batch and a bad one and ensure that batch-to-batch consistency (in terms of drug product performance) is maintained throughout the product’s lifecycle including any changes that may occur to the formulation post approval. The USP General Chapter <1092> The Dissolution Procedure has captured many of the steps required for development and validation of dissolution methods and is an excellent resource.
Gryczke (BASF): Firstly, the purpose needs to be determined--whether it is a QC method, one that measures pharmacokinetic performance, or both at the same time. Secondly, it has to be decided if all the different critical test parameters will be assessed in one method or if separate tests for particular aspects needs to be developed.
As an example, for lipid-based formulations of poorly soluble APIs, the specific aspects of enzymatic degradation, supersaturation (high kinetic solubility), and potential precipitation of the API from supersaturated state all need to be considered. One solution to investigate the dissolution and drug release is to use a multi-compartment model (acceptor-phase and donor phase). The sample is retrieved with the complex matrix of free fatty acids, bile salts, and pancreatin, for example. The API is then separated from the matrix by HPLC to determine the API concentration in the different phases of the release process. For daily use in a normal lab, this approach is quite a complex model although still manageable.
Conclusion
As discussed, there are several approaches and techniques used in dissolution testing, but it important that key considerations such as the API, formulation, and methodology are taken into account when designing a dissolution test.
Reference
1. Kostewicz et al., Eur. J. Pharm. Sc. 57, 342-366 (2014).
Article Details
Pharmaceutical Technology
Vol. 41, No. 6
Pages: 48–52, 68
Citation
When referring to this article, please cite it as A. Siew “Understanding Dissolution Testing,” Pharmaceutical Technology 41 (6) 2017.
Articles in this issue
over 8 years ago
Control Box Connects Lab Sensors and Pumpsover 8 years ago
Planetary Dispersers with PLC Recipe Controlsover 8 years ago
Paperless Recorder Shortens Sampling Intervalsover 8 years ago
Sterilizer Uses Pulsed Light Technologyover 8 years ago
Boosting Bioproduction Workflows with Automation Technologiesover 8 years ago
Decoding Serialization Regulationsover 8 years ago
Synchronizing Anticounterfeiting Effortsover 8 years ago
New and Updated Laboratory Equipment Optimize Efficiencyover 8 years ago
Particle Size Reduction for Investigational New DrugsNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.