Novartis' US Influenza Cell-Culture Facility Recognized
For its use of innovative technology for the production of seasonal and pandemic influenza vaccines, the Novartis Holly Springs, North Carolina facility was the Overall Winner of the 2013 Facility of the Year Award issued by the International Society for Pharmaceutical Engineering (ISPE).
The International Society for Pharmaceutical Engineering (ISPE) Facility of the Year Awards (FOYA) program recognizes state-of-the-art pharmaceutical manufacturing projects that use new and innovative technologies to enhance the delivery of quality products and reduce the cost of producing high-quality medicines. It also spotlights the accomplishments, shared commitment, and dedication of individuals in companies worldwide to innovate and advance pharmaceutical manufacturing technology for the benefit of all global consumers.
Novartis was recognized with the overall FOYA award in 2013 because its influenza cell- culture technology is a significant departure from the traditional approach to flu vaccine production, which relies on the growth of the virus in eggs. Cell-culture technology enables the use of raw materials that are readily available and not threatened by pandemic events, as well as closed-system bioreactors that reduce the required biosafety level for the manufacturing space. In addition, it is possible to provide rapid response to potential pandemic influenza threats while fulfilling the need for seasonal influenza vaccines.
First step: facility construction in partnership with HHS
Following the 2009 outbreak of the H1N1 pandemic flu and the numerous delays in producing vaccines against the virus, the US Department of Health and Human Services (HHS) recognized the need to invest in new vaccine technologies that can ensure national preparedness for a pandemic influenza or other diseases.
The dedication of the Novartis Holly Springs flu cell-culture plant in November 2011 was a first step in increasing the level of preparedness. Development of the cell-culture technology was funded in part by the HHS Office of the Assistant Secretary for Preparedness and Response, Biomedical Advanced Research and Development Authority, under Contract No. HHSO100200600012C. Construction of the Holly Springs facility was also funded in part by the same HHS agency under Contract No. HHSO100200900101C. The total public/private investment in the technology development and facility was more than $1 billion, according to Novartis. HHS and Novartis have committed to maintaining the facility under a public–private partnership for at least 25 years.
The Holly Springs facility has the capability to produce seasonal flu cell-culture vaccine, prepandemic vaccine, and 150 million doses of pandemic vaccine within six months of an influenza pandemic declaration, according to Novartis. A fill–finish set up for the production of both flu and non-flu products has also been installed in the facility.
Second step: FDA approval of cell-culture vaccine
Novartis received FDA approval for Flucelvax, the first cell-culture vaccine in the US designed to protect against seasonal influenza in individuals 18 years of age and older, in November, 2012. Clinical trial results indicated that Flucelvax was well tolerated with an acceptable efficacy against antigenically-matched strains and WHO-identified strains of the influenza virus compared to placebo for people aged 18 and older. Adverse reactions were found to be similar to those observed with the administration of other seasonal influenza vaccines (1).
Third step: first shipments of seasonal flu cell-culture vaccine
The first shipments of the cell-culture flu vaccine Flucelvax were made in August, 2013, along with shipments of the company’s conventional Fluvirin vaccine. The majority of shipments were completed in October in advance of the peak of influenza season. “We are pleased to offer a portfolio of flu vaccines that includes Flucelvax, which reflects how we are rethinking flu vaccination with a new approach to vaccine production and which offers a choice to consumers,” says Brent MacGregor, president of US Vaccines and Head of Region North America, in a press release.
Cell-culture vs. egg vaccine technology
Traditional vaccine manufacture begins with a ‘seed” virus identified and provided by the Centers for Disease Control and Prevention. This virus is introduced into fertilized chicken eggs. It then reproduces and builds up in the white (the allantoic fluid) of the egg, which is collected and purified. It takes two eggs to generate enough vaccine for one dose, and thus large numbers of eggs must be produced in advance of vaccine, which is always a challenge. Another difficulty with this approach is the fact the seed virus is not always accurately replicated, and as a result the virus in the vaccine may not be the same as the infective strain, and thus provides reduced immunity. Extensive DNA and protein analysis is required to help avoid this problem, and further testing is conducted to ensure that no pathogens from the eggs are transferred to the vaccine. All of this testing extends the production time and increases manufacturing cost.
Cell-culture vaccine advantages
The limited availability of eggs prevents the rapid production of vaccine, which is a major concern in a pandemic situation. It takes, in fact, many months to organize egg supplies, incubate the virus, obtain produced vaccine that can be delivered, according to Novartis.
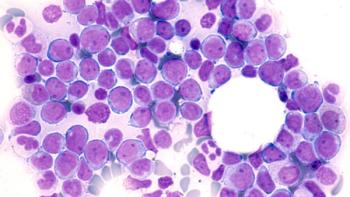
That is where cell-based flu culture has the advantage. Typically immortalized canine kidney cells are employed, and these cells can be stored in advance until needed and then rapidly amplified, enabling the production of large quantities of vaccine in a much shorter period of time than is possible using fertilized eggs. Cell-culture technology also enables more robust virus production, and therefore the virus in the vaccine is more consistent and more closely resembles the seed strain, which can be increased efficacy. In addition, the size of the bioreactors required to produce large numbers of doses is much smaller than the space required to produce a similar number of doses using eggs. Furthermore, the use of bioreactors ensures a closed, sterile, controlled environment, and thus the risk of potential impurities is reduced. As a result, Novartis’ Flucelvax vaccine does not contain any preservatives, such as thimerosal, or any antibiotics. Finally, unlike vaccines produced in fertilized eggs, cell-culture-derived vaccines can be administered to patients who are allergic to eggs.
Reference1. Novartis, "Flucelvax Package Insert," 2012.
Newsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.




