- Pharmaceutical Technology-01-02-2019
- Volume 43
- Issue 1
The Solubility Conundrum
Early adoption of the right approach to address solubility can deliver significant benefits.
Currently, a significant proportion of drugs that are approved or in the development pipeline are poorly soluble (1). This proportion may proliferate further as a result of the increasing drive to develop new chemical entities (NCEs) that are molecularly more complex.
Yet, despite offering noteworthy advantages-high selectivity and specificity, for example-more complex molecules also incur their own set of disadvantages. “As drugs become more complex, there is a trend towards higher molecular weight and increased lipophilicity that can decrease aqueous solubility,” confirms Jessica Mueller-Albers, strategic marketing director for oral drug delivery solutions at Evonik.
Julien Meissonnier (vice-president, Science and Technology) and Ronak Savla (scientific affairs manager), both from Catalent Pharma Solutions, agree that increasing molecular complexity impacts a drug’s solubility. “However, solubility is a deceptively complex phenomenon, and its minutiae can lead to different conclusions,” they add. “On the surface, it is simply dissolution of a solute (drug molecule) in a solvent (buffer or media). But, there are dozens of factors that affect solubility.”
Solubility of a substance happens under dynamic equilibrium (2), which means that dissolution and precipitation happen both simultaneously and in an opposing fashion. Therefore, it can be reasoned that intermolecular interactions between the solute (or drug) and solvent must be a consideration along with environmental factors, such as temperature and pressure.
“The factors considered to have the most influence are molecular descriptors such as molecular size, shape, flexibility, and hydrogen-bonding ability,” say Meissonnier and Savla. “A drug’s solubility is also greatly affected by the composition of the solvent system (pH, nature, strength of drug-solvent attractions), which is often underestimated when using aqueous solubility as an indicator for a drug’s solubility in biological conditions.”
Oral ingestion-the importance of permeability
Irrespective of route of administration, pharmaceutical drugs need to be in solution form in order to be absorbed (3), however, considering that the majority of drugs sold in the United States and Europe are administered orally (2) then intestinal permeability is also important. “Solubility, along with permeability, are the two most important factors affecting oral drug absorption and underlying the Biopharmaceutics Classification System (BCS) and Developability Classification System (DCS),” say Meissonnier and Savla.
BCS and DCS are classification systems used to predict what will impact the in-vivo performance of drugs (4,5). Predictions performed with these systems are restricted using solubility and permeability as parameters (2). Drugs are considered to be highly soluble when the highest-dose strength is soluble in 250 mL (or less) of aqueous solution (according to the BCS) or when the highest total dose in 500 mL (or less) of aqueous buffer pH 6.5 (according to the DCS).
However, for pharmaceuticals, the solvent of choice is water, in which most drugs are poorly soluble (2). Solubility, being the most important rate-limiting parameter for orally administered drugs, is a major challenge for the formulation scientist. “The increasing numbers of poorly soluble NCEs increase the importance of bioavailability enhancing technologies to enable development success,” add Meissonnier and Savla.
Overcoming solubility challenges
Solubility improvements can be achieved through several means, which fall under two main categories. “The two main methods to alter the solubility or dissolution of a drug substance are through either material engineering or formulation development,” says Mueller-Albers. “A mix of competencies that can be tailored to the specific needs of a project, including particle engineering, milling, solid dispersions, silica technologies, and formulations that enable rapid disintegration can be leveraged to enhance the solubility and bioavailability of drugs.”
An initial step in tackling solubility challenges for Meissonnier and Savla is optimization of the drug molecule itself through chemical design, followed by evaluation of the physical form of the molecule and its impact on solubility. “Despite these efforts, a growing number of molecules reach the preclinical and clinical development stage with persisting solubility issues, requiring advanced formulation technologies,” they add. “Several formulation technologies are designed to resolve solubility issues.”
However, they note that only a few of these formulation technologies demonstrate all the criteria desirable in drug development that can be used throughout clinical development and commercialization.
Formulation considerations
“First and foremost, formulating a poorly soluble molecule requires an in-depth characterization of its underlying bioavailability challenge,” stress Meissonnier and Savla. “Way too often, formulation scientists jump on the solubility challenge and try to resolve a partially defined or wrongly defined problem.”
For example, they explain, if trying to improve solubility of a formulation when the issue actually lies with dissolution rate, chemical instability, and/or high first-pass metabolism, time and effort could be wasted on the wrong development pathway. “The most important consideration revolves around employing the right models to characterize the molecule’s developability problems,” they continue. “It is key to leverage and develop the right physiologically based pharmacokinetic (PBPK) models to evaluate if the absorption hurdle is only solubility based. According the Biopharmaceutical Drug Disposition and Classification System (BDDCS), most poorly soluble and highly permeable drugs are subject to liver metabolism, and in several instances, drug metabolism at the gut wall and in the liver may be the main hurdles.”
Using the DCS, formulators can determine whether dissolution kinetics (DCS IIa) or intrinsic solubility (DCS IIb) is the main hurdle. If solubility is the main hurdle to formulation success, then leveraging the right model to bridge drug-substance properties with formulation technology becomes critical, according to Meissonnier and Savla. “One of the most important features of the DCS model is factoring in the total dose in relation to solubility,” they say. “In the very first animal studies, drugs are often tested at 10s–100s of milligrams per kilogram of body weight, which magnifies the solubility hurdle and may suggest the selection of the most complex technologies, whereas more simple solutions would be required for human clinical studies.”
There are numerous solubility enhancing technologies available, and for companies developing innovative drugs, selecting the best technology can be a difficult process. “Among many technologies, only a few have made it successfully to the clinic, and on to market. For DCS IIa molecules, particle size reduction (micronization and co-micronization) can overcome the slow dissolution rate, and for DCS IIb molecules, only lipid-based formulations and amorphous dispersions (made via spray drying and hot melt extrusion) have demonstrated commercial success,” explain Meissonnier and Savla. “Therefore, parallel screening of those technologies to select the most appropriate to the development stage is key.”
Mueller-Albers also notes the importance of a parallel approach. “It’s recommended to use predictive tools that can minimize development costs, as well as process technologies and equipment that avoid interactions with the API, enable higher drug loadings, and improve stability,” she says. “Finally, it’s always important to review the physical properties of the drug, ease-of-manufacturing, and the patent position.”
Dissolution testing
“A fundamental goal of pharmaceutical development is to optimize drug levels available in the body to match the therapeutic window, so that the desired therapeutic effect is achieved without adverse side effects,” Mueller-Albers states. “The effectiveness of any oral dosage form depends upon the intrinsic ability of the drug to reliably dissolve in the fluids of the gastrointestinal tract prior to it being absorbed into the blood stream. The rate of dissolution is a critical factor in this process.”
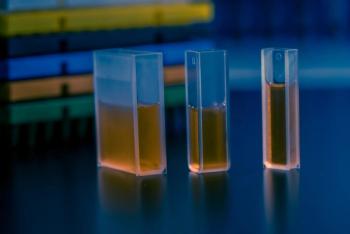
An important tool used within the pharma industry to determine the performance of oral solid dosage forms is that of dissolution testing (6). “Dissolution testing is a standardized method for measuring the rate of drug release from a given dosage form to optimize the formulation,” adds Mueller-Albers. “Tests must not only be robust and reproducible, but be able to detect any key changes in product performance between different formulations or batches. It is also essential that in-vitrodissolution matches in-vivo conditions. If the dissolution procedure is well designed, it should help to accelerate drug development by an effective selection of prototype formulations and de-risk the clinical studies, which are necessary in the drug product approval process.”
Meissonnier and Savla say that the first step should be to establish whether the dissolution testing is intended to be used to predict in-vivo performance or for quality assurance/control (QA/QC). “There are guidance documents and guidelines published by regulatory authorities and scientific organizations that deal with scale-up and post-approval changes, bioequivalence, and biowaivers,” Meissonnier and Savla continue. “A design of experiments (DoE) approach should be applied to develop a control strategy and define a design space. The API solubility and stability in the dissolution media should be part of the test set-up. Part of the dissolution test validation should assure that other components (i.e., excipients) do not interfere with ultraviolet absorbance, and that the calibration curve is linear and covers the lowest to highest concentration achieved during testing.”
When specifically looking at development projects involving poorly soluble drugs, Mueller-Albers explains that biorelevant media, such as fasted (FaSSIF) or fed-state simulated intestinal fluid (FeSSIF), can be employed. “These media contain solubilizing ingredients such as bile salts and phospholipids at physiological concentrations that are more precise in simulating the in-vivo solubility and dissolution rate of poorly soluble compounds than pure buffer media,” she says. “Dissolution volumes used in the in-vitro test can also be adapted to better reflect the physiological situation. Dissolution testing for QC purposes may also require a non-physiological pH, or the addition of solubilizers, such as sodium lauryl sulfate, to enable different product qualities to be differentiated based on the dissolution behavior.”
Conclusion
“Poor solubility was once considered to be a ‘show-stopper’ in formulation development,” summarizes Mueller-Albers. “However, while the risk of solubility has been reduced, there are still many drug candidates with physical characteristics that are incompatible with conventional processing technologies. Despite many pharmaceutical companies establishing standard processes for the development and manufacturing of drug products with poor solubility, in my opinion, there is still a strong need to select development partners that can provide rapid, reliable support into clinical studies.”
Considering oncology, Meissonnier and Savla state that this trend of compounds reaching patients with unaddressed solubility issues is magnified as clinical development pathways are often accelerated, leading to the first formulation that is investigated making it through to market launch. “So, poorly soluble oncology molecules (e.g., most protein kinase inhibitors) can reach the market with sub-optimal formulations and persistent solubility shortcomings,” they note.
If these solubility issues are not addressed, there may be dire consequences. “Solubility issues may result in higher pharmacokinetic variability (intra- and inter-patient) and a positive food effect (sometimes translated into a marked increase in serum concentrations of tenfold or higher). These detrimental properties, often combined with a narrow therapeutic index, can lead to significant challenges in patients and avoidable black box warnings,” Meissonnier and Savla warn. “Therefore, the early adoption of the right formulation technology to address poor solubility can deliver significant patient benefits and complement market differentiation.”
References
1. S. Kalepu and V. Nekkanti, Acta Pharmaceutica Sinica B, 5 (5) 442-453 (2015).
2. K.T. Savjani, A.K. Gajjar, and J.K. Savjani, ISRN Pharmaceutics, 2012 Article ID 195727 (2012).
3. A. Chaudhary et al., J.Advanced Pharmacy Education & Research, 2 (1) 32-67 (2012).\
4. L.Z. Benet, J. Pharm. Sci.,102 (1) 34-42 (2013).
5. J.M. Butler and J.B. Dressman, J. Pharm Sci.,99 (12) 4940-4954 (2010).
6. A. Siew, Pharm. Tech., 40 (11) 56-64 (2016).
Article Details
Pharmaceutical Technology
Volume 43, Number 1
January 2019
Pages: 48–51
Citation
When referring to this article, please cite it as F. Thomas, "The Solubility Conundrum," Pharmaceutical Technology 43 (1) 2019.
Articles in this issue
about 7 years ago
Packaging Peril: ‘No-Deal’ Brexit May Lead to Missed Deadlineabout 7 years ago
Looking Beyond the Deadlineabout 7 years ago
Great Expectationsabout 7 years ago
Smarter Packaging Comes to the Pharma Marketabout 7 years ago
Improved Mixer Lift and Seal Designsabout 7 years ago
Tabletop Spray Dryerabout 7 years ago
Microplate Spectrophotometerabout 7 years ago
Electrical Position Indicator for Linear Actuatorsabout 7 years ago
FDA Marks Record Year for New Drug ApprovalsNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.