- Pharmaceutical Technology-03-02-2020
- Volume 44
- Issue 3
Going with the Flow
Metrology has the potential to not only prevent harm to patients but also to support innovative therapeutic options.
Editor’s Note: This article was published in Pharmaceutical Technology Europe’s March 2020 print issue.
The pharmaceutical industry is estimated to contribute billions to the European economy and provides employment to millions of people across the region (1). Additionally, the industry induces benefits to the region’s overall economy significantly through improved health and the resultant increased life expectancy of the working population (1).
Bringing innovative therapies to market has been well-documented as being expensive and time-consuming (2), leading bio/pharma companies to seek out ways in which they can be more efficient during drug development. “Metrology has an essential role to play in drug development and delivery to provide the certainty that leads to safety, quality, and efficacy with each infusion, tablet, or capsule,” says Dr. Tracy Brown, head of life sciences at TÜV SÜD National Engineering Laboratory. “Establishing robust metrological infrastructures specific to the development of new API formulations and administration of the final dosage form to patients ensures traceable, accurate, and reproducible measurements that will expedite ‘idea to invoice’ and clinical uptake.”
Underestimated risks of infusion
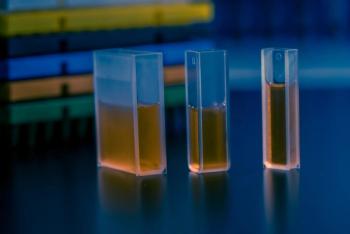
A common route of drug delivery is via infusion, which is a particularly suitable delivery method for drugs that need to be rapidly absorbed or for drugs that are highly toxic and need to be administered in small doses continuously. For this type of administration, the flow rate of the drug is an important parameter to ensure accuracy (3).
“It is crucial that the physicochemical (e.g., solubility, density, viscosity) and flow properties (rates, pressures) of the drug formulation (API and excipients) being developed for intravenous infusion are measured to ensure safe and efficacious drug delivery,” Brown confirms. However, some published studies have highlighted an underestimated risk with infusion administration (4–7). For example, an inadequate amount of drug being administered leading to adverse reactions. “Infusion errors can lead to adverse incidents and, at worst, prove fatal,” Brown stresses.
Additional complications may arise from the use of multiple infusion systems, Brown continues. “Multi-infusion systems require additional metrology to determine how the mixing and flow of liquids with differing viscosities affect drug concentration both within the infusion lines and at the outlet of the infusion device,” she says.
Specific patient populations may also require further contemplation. “Infusions in certain patient groups (e.g., neonates) demand very low flow rates in the nanolitre (nL) per minute range placing greater challenges for dosing accuracy and reliability,” Brown adds.
Furthermore, it is important to consider the primary packaging and different devices that are incorporated into infusion systems. “In the case of intravenous administration, for example, various devices with differing purposes may be used (syringe pumps, peristaltic pumps, insulin pumps),” Brown notes. “There have been advances in using microneedles in patches applied to the skin as a more effective and painless way to deliver drugs to patients. Each method must be capable of delivering traceable, accurate, and reproducible metered doses of drug. Therefore, understanding the sources of, and minimizing, measurement uncertainties attributable to the operation of each device is key.”
European project
In 2012, a joint research project, funded by the European Metrology Research Programme (EMRP), was undertaken with the aim of developing traceable calibration services for drug delivery of flow rates down to 1 nL per minute, assessment methods for drug delivery devices, and a best practice guide (8). The first project was successfully completed in 2015 and has led to a follow-on project-Metrology for Drug Delivery (MeDD) II-being launched in June 2019 (8).
“A European consortium of National Measurement and Designated Institutes, universities, and manufacturers have embarked upon a three-year project (MeDD II) aimed at improving dosing accuracy and enabling the traceable measurement of volume, flow, and pressure of drug delivery devices used in infusion therapy,” says Brown. “This research will enhance the pharma industry’s understanding of the most common form of therapy and be of particular significance given the increasing complexity of many new active drug candidates.”
An additional aspect of this project will investigate how mixtures of liquids with differing viscosities mix and flow in multi-infusion systems, Brown reveals. “Additionally, the effect that this mix of liquids may have on the therapeutic drug concentration during the course of the infusion will be examined,” she adds. “Such rigorous metrology will prevent harm to patients arising from inappropriate mixing such as therapeutic failure or toxicity.”
Continuous manufacturing
“Continuous manufacturing has the potential to transform medicine production,” says Brown. “This alternative approach to traditional batch methods holds great promise for the pharma industry in reversing the trend of diminishing returns on R&D investment. Lower costs and faster production times coupled with reduced physical and environmental footprints and improved quality make an attractive proposition.”
The potential of continuous manufacturing has been recognized within Europe. Using the United Kingdom as an example, Brown highlights the investment that is being made by the government and industry to create research and innovation centres, such as the Centre for Process Innovation (CPI) and Medicines Manufacturing Innovation Centre (MMIC). “These hubs aim to develop innovative continuous manufacturing technologies with the flexibility and scalability to clinical trial and commercial volumes,” she adds.
Despite the potential advantages offered by continuous manufacturing, its uptake within the bio/pharma industry has been slow. The seeming reluctance by the industry to adopt continuous manufacturing has been attributed to multiple factors, such as regulatory and operational challenges (9). Additionally, an understanding of the process and dynamics that will be affected by continuous manufacturing is required for successful implementation (10).
“In addition to knowledge of production technology and process engineering, it is recognized that effective flow measurement science and standards development will play an important role in bringing continuous manufacturing to life,” emphasizes Brown. “For example, the calibration and validation of process analytical technology for inline, realâtime quality control.”
Fundamental changes and exciting opportunities
Given the increasing prevalence of personalized medicines, the delivery of drugs is expected to fundamentally change and, as Brown explains, is predicated on the idea that different sizes of dose can be accurately delivered. “The journey towards therapeutic and prophylactic interventions tailored to individuals that take into account their genetic blueprint, environment, and lifestyle is underway,” she says. “Intrinsically, this will necessitate the need for enhanced metrological capability to ensure the accurate dosing of infusions containing novel complex therapeutics designed to treat niche illnesses.”
Regulatory standards will also be required to be updated to address the diversity and increasing complexity of novel therapeutic solutions, such as personalized medicines. “Regulatory compliance underpins every innovation or innovative methodology within medicines and healthcare products,” Brown confirms. “A characteristically judicious approach will inevitably see regulators seeking to require drug developers and medical device manufacturers to apply metrological standards at national, European, and international level to new discoveries.”
Other exciting opportunities for drug development include the microfluidic technologies that are rapidly evolving, Brown notes. “Organ-on-a-chip is a microscale in-vitro model that can be used for simulating the pharmacologic effects of new drug candidates on complex biological processes. It is efficient and cost-effective with the potential to reduce reliance upon the use of animal models,” she says. “Fluid flow measurement will be important in these novel microfluidic applications and necessary to ensure their continuing maturity and impact.”
References
1. EFPIA & PwC, “
2. J.A. DiMasi, H. G. Grabowski, and R.W. Hansen,
3. P. Lucas and S. Klein,
4. D. Capes and R. Kimble,
5. J.I. Westbrook, et al.,
6. R.A. Peterfreund and J.H. Philip,
7. A. Vijayakumar, et al.,
8. MeDD, “Metrology for Drug Delivery,” drugmetrology.com [accessed 17 Feb. 2020].
9. S. Milmo, Pharm. Tech. Eur., 29 (11) 8–9 (2017).
10. R.S. Chaudhary, A. Pazhayattil, and J. Spes, “Continuous Manufacturing: A Generic Industry Perspective,” PharmTech.com, Online Exclusive, 30 May 2017.
Article Details
Pharmaceutical Technology Europe
Vol. 32, No. 3
March 2020
Pages: 32–33
Citation
When referring to this article, please cite it as F. Thomas, “Going with the Flow,” Pharmaceutical Technology Europe 32 (3) 2020.
Articles in this issue
almost 6 years ago
Drug Production Draws Multiple Contendersalmost 6 years ago
Coronavirus Response: Reaction or New Reality?almost 6 years ago
Embracing Change Managementalmost 6 years ago
Double Planetary Mixeralmost 6 years ago
Isolator Head for Microbial Air Samplingalmost 6 years ago
Compressor-Free Plate Sealeralmost 6 years ago
Double Clamshell Barrel Continuous Processoralmost 6 years ago
Challenges in Clinical Manufacturing for Topical Drugsalmost 6 years ago
Stability Testing: The Crucial Development Stepalmost 6 years ago
Keeping Toxicity to a MinimumNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.