Pharmaceutical Technology Europe
- Pharmaceutical Technology Europe-03-01-2009
- Volume 21
- Issue 3
LC–MS/MS method for the determination of Vitamin D3 in human plasma
An LC–MS/MS method for the quantitative determination of vitamin D3 in human plasma has been developed and validated with positive atmospheric chemical ionization sources.
Vitamin D comprises a group of secosteroids, and mainly refers to two physiologically inactive fatsoluble prohormones: vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol). Vitamin D3 is photochemically synthesized from 7dehydrocholesterol in the epidermal layer of the skin of vertebrates under ultraviolet (UV) B light (270–290 nm) radiation. Vitamin D2 is derived from fungal and plant sterol when ergosterol is exposed to UV radiation. Vitamin D2 is not produced by the human body and is much less effective than vitamin D3 in humans.1
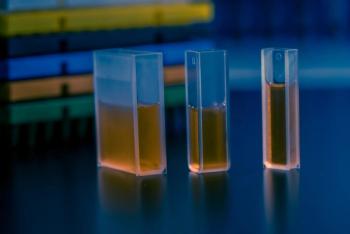
(Nick Koudis/Getty Images)
The metabolic pathways of vitamins D3 and D2 in humans are similar. Vitamin D3 is hydroxylated in the liver and converted to a nonactive storage form of 25hydroxycholecalciferol, which is further metabolized in the kidneys into the physiologically major active hormone, 1,25dihydroxycholecalciferol. This hormone is the main circulating form of vitamin D, which enhances the ability of the small intestine to absorb calcium and retain phosphate from the diet, and prevents metabolic bone diseases such as rickets, osteomalacia, osteoporosis and agerelated macular degeneration,2,3 which are caused by vitamin D deficiency.
In 2007, the Canadian Cancer Society recommended that adults living in Canada should consider taking vitamin D supplements of 1000 IU/day during the autumn and winter, and those at higher risk of lower vitamin D levels should take 1000 IU/day all year round.4 Meanwhile, the US Dietary Reference Intake for Adequate Intake of vitamin D3 lists: 200 IU/day as adequate for children and adults aged ≤50 years, 400 IU/day for adults aged 51–70 years, and 600 IU/day for adults aged >71 years.5
Fifteen experts from universities, research institutes and university hospitals worldwide called for international agencies, such as the Food and Nutrition Board (WA, USA) and the European Commission's Health and Consumer Protection DirectorateGeneral (Belgium), to reassess dietary recommendations for vitamin D as a matter of high priority because the formal advice from health agencies is outdated and putting the public at risk.6 Currently, the FDAapproved prescription oral tablet drug FOSAMAX PLUS D (70 mg alendronate sodium/5600 IU cholecalciferol) has been widely used for people diagnosed with osteoporosis. Alendronate slows bone loss and increases bone mass, which helps prevent bone fractures, while cholecalciferol aids bone absorption of calcium.
Levels of vitamin D3 and its metabolites, 25hydroxyvitamin D3 and 1,25dihydroxyvitamin D3, are usually clinical indicators of nutritional vitamin D deficiency in humans.7,8 Based on FDA guidance for bioavailability and bioequivalence studies for orally administered drug products, the moieties to be measured in biological fluids collected are either the API or its active moiety in the administered dosage form (parent drug) and, when appropriate, its active metabolites.
For bioequivalence studies, measurement of the concentration–time profile of the parent drug released from the dosage form, rather than the metabolite, is generally recommended because it is more sensitive to changes in formulation performance than metabolites.
Measurement of a metabolite may be preferred when parent drug levels are too low to allow reliable analytical measurement in blood, plasma or serum for an adequate length of time, or when a metabolite may be formed as a result of gut wall or other presystemic metabolism.9 Therefore, it is of more clinical importance to directly monitor vitamin D3 levels in the human body when a vitamin D drug or a supplement is taken.
Previous determination of endogenous vitamin D has mainly been conducted by high performance liquid chromatography/ultraviolet (HPLC/UV) and gas chromatography/mass spectrometry (GC/MS) methods. These methods were considered challenging because their low sensitivities for low vitamin D levels in circulation required highblood volumes. The similarity between vitamin D and its analogs and metabolites meant that HPLC methods suffered from inadequate chromatographic separation and lacked specificity of interference. The dynamic endogenous concentration of vitamin D in the presence of UV light, and complex labourintensive and timeconsuming sample extraction procedures from ligand binding assays and low recovery from derivatization methods were also problematic.10–12
LC–MS/MS methods have been widely used for the determination of vitamin D3 metabolites and analogs, but not very much for the direct determination of endogenous vitamin D3 in human plasma.13
This paper presents an atmosphericpressure chemical ionization (APCI)LC–MS/MS method developed and validated to accurately measure the absolute quantities of endogenous vitamin D3 in human plasma.
Chemicals
Cholecalciferol was purchased from Sigma Aldrich (Canada) and hexadeuterated (d6)-vitamin D3 was purchased from Chemphor Inc. (Canada). Blank human plasma with dipotassium ethylenediaminetetraacetic acid (EDTA) anticoagulant was received frozen on dry ice from Bioreclamation Inc. (NY, USA). Methanol (HPLC grade) and acetonitrile (Omnisolv grade) were from EMD (NJ, USA). Formic acid (ACS grade) was from Fisher Scientific (Canada) and deionized water was prepared in a Millipore (France) water system (MilliQ Gradient Ultrapure).
Equipment
An MDS/Sciex API5000 triple quadrupole mass spectrometer (MDS Sciex, Canada) interfaced with an APCI source (MDS Sciex) coupled with an Agilent 1100 series thermostatted column compartment (Agilent Technologies, Switzerland), a binary pump (Agilent Technologies), a degasser (Agilent Technologies), a Leap Technologies' (Switzerland) CTC analytics LC PAL series autosampler, and a VICI (TX, USA) valco valve, was used and controlled by Analyst (Applied Biosystems, MA, USA).
LC was conducted on a Zorbax Eclipse XDBC8 column (Agilent Technologies, USA) (50 × 4.6 mm, 3.5μm) maintained at 25 °C. A total of 20 μL of each sample was injected onto the column. The mobile phase operated at a flow rate of 1200 μL/min and consisted of 0.1% (v/v) formic acid in water as solvent A and methanol as solvent B under gradient elution.
Sample preparation
Stock and working solutions of vitamin D3 and internal standard, d6-vitamin D3, were prepared in methanol and stored at –40 °C. A sufficient amount of frozen inhouse prepared surrogate human plasma was thawed.
Quality control samples at 0.25 ng/mL (QC-LOQ), 0.75 ng/mL (QC-L), 6.00 ng/mL (QC-M1), 12.50 ng/mL (QCM2) and 18.00 ng/mL (QC-H) were prepared in surrogate human plasma, aliquoted in small volume vials and stored at –40 and –70°C for stability assessment.
Calibration standards with a range of 0.25–25.00 ng/mL were freshly prepared daily in surrogate human plasma. Vitamin D3 samples (200 μL aliquots) were prepared using a protein precipitation method. After precipitation, the supernatant layer was transferred, evaporated to dryness under nitrogen gas and the residue was redissolved with 150 mL of methanol:water mixture.
Optimization of MS/MS parameters
Vitamin D3 is a white crystalline powder soluble in 100% ethanol, chloroform or acetone and insoluble in water. It is light sensitive and should be protected from exposure to light. The stable isotopelabelled d6-vitamin D3 was used as an internal standard for quantitation of vitamin D3 (Figure 1). The electrospray ionization source (ESI) showed very low sensitivity to vitamin D3 and its internal standard because of the lack of protonation sites on the fatsoluble vitamins, making their ionization very difficult. The relatively stable structure of vitamin D3 gives few fragment ions.
Figure 1: Structures of vitamin D3 and its internal standard, d6-vitamin D3.
APCI, previously found to be a suitable ionization source for the characterization of steroids, was used for vitamin D3.14 Although the product ions of m/z 367.2 from vitamin D3 and m/z 373.2 from d6-vitamin D3 show relatively stronger signal intensity than those of m/z 259.2 and m/z 265.2, the former were not used because they are the fragment ions of the parent molecular ions after losing one water molecule ([M + H-H2O]+).
Significant matrix interference was also observed in later chromatographic separation when using m/z 367.2. Optimal multiple reaction monitoring (MRM) transitions at m/z 385.2–259.2 for vitamin D3 and m/z 391.3 to 265.2 for d6-vitamin-D3 were selected.
Selection of surrogate matrix
Vitamin D3 is an endogenous component in human plasma reported in the range 0.7–5.7 ng/mL10 and 19.74 ± 9.48 ng/mL.11 Endogenous vitamin D3 in humans is dynamically changed daily, with its skin biosynthesis affected by multiple factors, such as altitude, sun exposure, clothing, season, ageing and skin melanin pigmentation.
FDA recommends that the same biological matrix as the samples in the intended study be used for the standard calibration curve, prepared by spiking the matrix with known concentrations and that the low limit of quantitation (LLOQ) response should be at least five times the response of a blank.9 However, it is impractical to prepare the standard calibration curves and quality control samples in human plasma because of the endogenous vitamin D3.
Proper selection of a surrogate matrix to establish a quantitative standard calibration curve and quality control samples for vitamin D3 for the range 0.25–25.00 ng/mL posed enormous challenges for the establishment of an effective bioanalytical method for the determination of endogenous vitamin D3 in human plasma. Different approaches in the selection of a surrogate matrix for determining endogenous components in biological matrices have been reported, such as preparation of calibration standards of seven endogenous ketolic estrogens in methanol instead of human urine;15 pretreatment of blank human nerve tissues instead of using normal human nerve tissue for determination of endogenous sorbitol and fructose;16 preparation of endogenous hormones in solutions of phosphate buffer and bovine serum albumin instead of human serum and urine to prevent contamination from various endogenous hormones;17 determination of endogenous estrogens using charcoalstripped human urine;18 and calculation of endogenous components using background substraction.
Various lots of charcoalstripped human plasma from different commercial sources were tested and evaluated and significant amounts of vitamin D3 were still observed in these custommade blank human plasma samples. Exposing the charcoalstripped blank human plasma samples directly to indoor light for 48 h did not reduce endogenous vitamin D3 levels.
Several other surrogate matrices, such as human serum, rat plasma and serum, mouse plasma and serum, and human and bovine serum albumin were also evaluated for the assay.19 The different surrogate matrices also affected vitamin D3 sample freeze and thaw stability.
An inhouse method developed to strip vitamin D3 from commercial blank human plasma using a charcoalstripping technique was successfully established. The charcoal particle size distribution, surface area, porosity, carbon percentage, and the treatment method of the activated charcoal were the keys to the successful preparation of quality vitamin D3free charcoalstripped human plasma.
For standards prepared in surrogate matrix 2 (Figure 2), the slope of the standard calibration curve was significantly lower for the extracted samples stored overnight at –40 °C than that of the extracted samples that were freshly prepared.
Figure 2: Effect of surrogate matrix on vitamin D3 standard calibration curves.
For surrogate matrix 1 (Figure 2), the slope of the standard calibration curve shows no significant difference between samples that were freshly prepared or frozen. Supplementary data (
Avoiding endogenous interference
Fat-soluble vitamin D3 is a highly hydrophobic compound that strongly retains onto the chromatographic column. Various brands and types of reversephase columns were tested and it was found that vitamin D3 could not be eluted from all tested C18 columns when using 100% methanol or acetonitrile for 15 min.
Reasonable retention time and good peak shape were achieved when using Synergy 4 μm Polar-RP 80 A° (50×4.6 mm, 4μm) (Phenomenex, USA) and Zorbax Eclipse XDBC8 (50×4.6 mm, 3.5μm) (Agilent Technologies, USA) columns. However, the vitamin D3 peak overlapped with the shoulder of the significant interference peak of an endogenous unknown when using the former column.
Two major interference peaks with retention times at 2.0–2.4 and 2.8–3.5 min were observed before and after the vitamin D3 peak (Figure 3a). Complete baseline separation of vitamin D3 from the endogenous interference peaks was obtained after further optimization of the LC elution gradient (Figure 3b).
Figure 3: Optimization of LC gradient to separate vitamin D3 from interferences.
Supplementary data (
Data online (
Sample extraction and storage
The poor water solubility and strong binding ability to globulin proteins in human blood make vitamin D3 very difficult to extract. Liquid–liquid extraction and protein precipitation methods were both tested for vitamin D3 sample preparation and found to obtain similar results.
The less labourintensive and costeffective protein precipitation method was used for sample preparation. To avoid vitamin D3 coprecipitation and improve extraction recovery, it is recommended to thoroughly mix and vortex before centrifugation.
The influence of the containers used for vitamin D3 preparation and storage was also investigated. Although no significant difference was observed for standard calibration curves prepared in either plastic or glass vials, the accuracy of QC-L, QC-M1 and 5-fold diluted samples prepared in glass vials was out of the acceptance criteria for QC samples (Figure 4).
Figure 4: Effects of vitamin D3 adsorption on (a) standard and (b) accuracy of quality control.
Severe adsorption of vitamin D3 onto the glass vials might have been the cause of the poor accuracy. The accuracy for all QC samples prepared in plastic vials was within the acceptance criteria range. Therefore, vitamin D3 sample preparation and extraction should be performed in plastic vials instead of glassware to minimize vitamin D3 adsorption onto the containers.
Precision, accuracy of QC
The LLOQ of the vitamin D3 assay was validated at 0.25 ng/mL in five validation batches. The intrabatch precision (% CV) and accuracy (%RE) at the LLOQ with the five validation batches ranged 3.1–5.5, and –4.2–3.0, respectively. The interbatch precision (%CV) and accuracy (%RE) at LLOQ calculated based on the mean of individual batch means, were 3.3 and –0.4.
The assay regression model was evaluated by analysing calibration curve samples in duplicate with the vitamin D3 concentration range 0.25–25.00 ng/mL. Quadratic regression (weighted 1/X2) was performed for each combined calibration standard curve with a mean correlation coefficient (mean±SD) of 0.9986 ±0.0004 (n=5). The interbatch precision of the assay (%CV) ranged 0.9–6.8. The interbatch accuracy (%RE) for backcalculated values ranged –3.6–5.2, indicating an acceptable goodness-of-fit.
Five replicates at each QC concentration level (QC-LOQ, QC-L, QC-M1, QC-M2, and QC-H) were analysed in each of the five validation batches to determine intra- and interbatch precision and accuracy of the method. No samples were excluded from the accuracy and precision statistics. The intrabatch precision (%CV) and accuracy (%RE) of the method ranged 0.5–5.5, and –8.0–7.1, respectively. The interbatch precision (%CV) and accuracy (%RE) ranged 1.9–3.5, and –5.5–1.2, respectively. The precision (%CV) and accuracy (%RE) of the 5fold diluted QC-HCON samples of 50.00 ng/mL were 1.4 and 7.9, respectively.
Assay recovery and matrix effect
Assay recovery for vitamin D3 was evaluated by comparing the peak area ratios of vitamin D3 to internal standard of extracted QC samples in five replicates of QC-L, QC-M1 and QC-H to peak area ratios of nonextracted analyte (control) samples. Control samples were prepared by extracting plasma samples containing internal standard and spiking the plasma extracts with vitamin D3 at concentrations calculated to be the same as those of the extracted QC samples, assuming 100% recovery. The mean assay recovery (mean±SD, n=5) of vitamin D3 from human plasma of QC-L, QC-M1 and QC-H was 46.6±6.2% (%CV of 13.4), 46.0±2.0% (%CV of 4.4) and 43.0±3.3% (%CV of 7.6), respectively. Overall mean assay recovery (mean±SD, n=15) was 45.2±4.2%.
Similarly, assay recovery for the internal standard was evaluated in five replicates of QC-L and QC-H. The mean assay recovery (mean±SD, n=5) of internal standard from human plasma was 50.2±1.9% (%CV of 3.8) and 50.4±3.1% (%CV of 6.2), respectively. Overall mean assay recovery (mean±SD, n=10) of internal standard was 50.3±2.4%. It was observed that assay recovery for both vitamin D3 and internal standard showed consistency at each level of test concentration with good precision and reproducibility.
The matrix effect on the ionization of vitamin D3 was evaluated in five replicates at QC-L, QC-M1 and QC-H by comparing the response (total peak area counts) of analyte spiked into plasma extracts to the response of analyte in neat solution (control) samples. Neat solutions were prepared by spiking with vitamin D3 at concentrations calculated to be the same as those of extracted QC samples, assuming 100% recovery, such that the neat solution concentrations match the recovery experiment control samples. The mean matrix effect (%) of QC-L, QC-M1 and QC-H was –6.4, –2.8 and –4.4, respectively. Overall mean matrix effect (%) was –4.5, indicating a negligible matrix effect. Similarly, the matrix effect on the ionization for internal standard was evaluated and the mean matrix effect (%) of QC-L and QC-H vitamin D3 concentrations was –10.6 and –9.7, respectively. Overall mean matrix effect (%) was –10.2, indicating a negligible matrix effect.
Matrix comparison of QC samples
The mean endogenous vitamin D3 concentration in different lots of unaltered human plasma pooled together was determined to be 5.81 ng/mL. The accuracy and precision of QC samples prepared in pooled unaltered human plasma at nominal concentrations of 6.00 ng/mL (NBQC-M1, effective concentration 11.81 ng/mL) and 12.50 ng/mL (NBQCM2, effective concentration 18.31 ng/mL) was assessed during assay validation.
The precision (%CV) of the QC samples prepared in unaltered human plasma at NB-QC-M1 and NB-QC-M2 was 1.0 and 1.7, respectively. The accuracy (%RE) of the QC samples prepared in unaltered blank human plasma at NB-QC-M1, NB-QC-M2 was 2.8 and –0.8, respectively. QC samples prepared in unaltered human plasma demonstrated acceptable precision and accuracy.
The % difference between the mean calculated concentration in surrogate and unaltered human plasma after adjustment for 5.81 ng/mL endogenous vitamin D3 in the unaltered plasma was 14.6 and 0.5 at QC-M1 and M2, respectively. Therefore, the surrogate human plasma and the unaltered human plasma matrices are comparable when used for vitamin D3 analysis.
Vitamin D3 stability
Drug stability experiments should mimic conditions under which samples are collected, stored and processed, as closely as possible. The experiments should be conducted in unaltered representative matrix, including the same type of anticoagulant. In cases where stripped or altered matrix is used for preparation of study calibration standards and/or QC samples, stability evaluation still must be conducted in samples prepared in unaltered matrix. If a stabilizer is normally employed with incurred samples, it should be employed with the stability samples as well.20
The endogenous vitamin D3 levels in different lots of unaltered human plasma were pre-screened and pooled together at two concentration levels, low pool and high pool. Storage stability was evaluated at –40 °C in five replicates of different vitamin D3 concentrations of QC-L and QC-H prepared in surrogate human plasma, and in high pool and low pool unaltered human plasma. Stability samples were compared with the mean measured concentration values of time zero QC samples in the initial batch (control). Vitamin D3 stability established in surrogate and unaltered human plasma included three freeze/thaw cycles, storage at ambient room temperature for 20 h, 3 days shortterm storage stability and 2 months (69 days) longterm stability for surrogate human plasma stored at –40 and –70°C, and unaltered human plasma stored at –70°C.
Vitamin D3 stock solution stability was established for 6 h at room temperature and after 2 months (71 days) storage at –40 °C. Standard solution samples were prepared at an equivalent concentration to QC-H and analysed by LC–MS/MS together with control samples prepared fresh at an equivalent concentration on the day of analysis.
Reinjection reproducibility
The reinjection reproducibility of extracted plasma samples in the autosampler tray was assessed at QC-L and QC-H. The extracts were stored at ambient room temperature on the autosampler tray and were repeatedly injected into the LC–MS/MS to establish reinjection reproducibility for up to 316 h.
Assay specificity and selectivity
Extraction and subsequent chromatographic analysis of six blank surrogate human plasma samples (obtained from different lots of surrogate human plasma) demonstrated that no significant interference from plasma constituents was observed at the retention times of the mass transitions for vitamin D3 or internal standard. The chromatographic analysis of six blank surrogate human plasma samples (obtained from different lots of surrogate human plasma) spiked with vitamin D3 at LLOQ and internal standard demonstrated that no interference from plasma constituents was observed at the retention time of the mass transitions for vitamin D3 or internal standard. No mass spectral interference was observed from the internal standard at the mass transitions for vitamin D3 when the internal standard was spiked alone as pure solvent sample or as an extracted surrogate human plasma sample. No mass spectral interference was observed from vitamin D3 at the mass transitions for internal standard when vitamin D3 was spiked alone as pure solvent sample or as an extracted surrogate human plasma sample.
System suitability
Duplicate injections of system suitability samples containing vitamin D3 at equivalent concentrations of QC-L and QC-H, and internal standard in reconstitution solution were analysed at the beginning and end of each batch. System suitability samples were used to qualify and properly maintain instruments to ensure the system was operating correctly at the time of analysis with sufficient sensitivity, specificity and reproducibility for the analytical run. An acceptable range of values for vitamin D3 system suitability established from method validation data will be applied for sample analysis.
Conclusion
A rapid, sensitive, specific, accurate and reliable APCI–LC–MS/MS analytical method for the determination of vitamin D3 in human plasma was developed and validated with a concentration range 0.25–25.00 ng/mL.
Xuejun Peng is Laboratory Manager at Can Test Ltd (Canada).
Rong Yi is a Senior Analyst at Can Test Ltd.
Amara Pinnawala is a Senior Analyst at Can Test Ltd.
Sarah Ostonal is an Analyst at Can Test Ltd.
Eliot Chung is an Analyst at Can Test Ltd.
Grace van der Gugten is a Senior Analyst at Can Test Ltd.
Bernard Nutley is a Senior Scientist at Can Test Ltd.
David Gray is Director of Specialty Services at Can Test Ltd.
References
1. L.A.G. Armas, B.W. Hollis and R.P. Heaney, J. Clin. Endocrinol. Metab., 89(11), 5837–5391 (2004).
2. J.M. Lapper et al., J. Am. Coll. Nutr., 25(5), 395–402 (2006).
3. J.M. Lappe et al., Am. J. Clin. Nutr., 85,(6), 1586–1591 (2007).
4. Canadian Cancer Society, (2007).
5. Institute of Medicine of the National Academies, Dietary Reference Intake (2008).
6. R. Vieth et al., Am. J. Clin. Nutr., 85(3), 649–650 (2007).
7. M.A. Preece et al., Clin. Chim. Acta., 54(2), 235–242 (1974).
8. B. Garcia-Pascual et al., Clin. Chim. Acta., 68(2), 99–105 (1996).
9. FDA Guidance for Industry — Bioavailability and Bioequivalence Studies for Orally Administered Drug Products — General Considerations, March 2003.
10. R.M. Shepard et al., Biochem. J., 182(1), 55-69 (1979).
11. M.R. Brunetto et al., Talanta, 64(5), 1364–1370 (2004).
12. M. Osadca and M.J. Araujo, Assoc. Off. Anal. Chem., 60(5), 993–997 (1977).
13.
14. A. Heudi, M.J. Trisconi and C.J. Blake, J. Chromatogr. A., 1022(1–2), 115–123 (2004).
15. X. Xu et al., Anal. Chem., 76(19), 5829–5836 (2004).
16. H.R. Liang et al., Rapid. Commun. Mass Spectrom., 19(16), 2284–2294 (2005).
17. C.A. Reilly and D.J. Crouch, J. Anal. Toxicol., 28(1), 1–10 (2004).
18. X. Xu et al., Anal. Chem. , 77(20), 6646–6654 ( 2005).
19. X. Peng and D. Gray, Laboratory Focus , 0227, 8–14 (July, 2007).
20. C.T. Viswanathan et al., AAPS Journal, 9(1), E30–42 (2007).
Articles in this issue
almost 17 years ago
Evaluating the pieces of the pharma supply chainalmost 17 years ago
Facilitating technology transfer to your CMOalmost 17 years ago
Building on the promise of biotechalmost 17 years ago
Goodbye and helloalmost 17 years ago
Predictive modelling: putting ICH guidelines to work in process validationalmost 17 years ago
PAT: HPLC on the horizon?almost 17 years ago
Quantifying experience in powder processingalmost 17 years ago
Ensuring raw material qualityNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.