- Pharmaceutical Technology's In the Lab eNewsletter, August 2021
- Volume 16
- Issue 08
Preparing for Unexpected Issues in E&L Studies for Biopharma
Establishing extractable and leachable studies for complex biotherapeutic molecules poses new challenges for analytical assessment.
Extractable and leachable (E&L) studies have become an integral part of any drug development program and serve to ensure compatibility between the product and its packaging. While such studies are now generally well defined in terms of experimental design and data evaluation, these have had to adapt to the ever-increasing diversity of therapeutic products. There are, for example, some unique challenges in the analysis of biopharmaceutical products as a result of certain formulation components, as well as the complexity of the therapeutic itself. This article describes a number of challenges and solutions in the E&L evaluation of biopharmaceuticals and highlights a selection of those encountered with emerging cell and gene therapy (CGT) products.
Ongoing E&L challenges
The risks posed by leachables on product quality and patient safety are an ongoing challenge for the pharmaceutical and biopharmaceutical industries. Continued investigational development in this area is primarily driven by a number of factors, including: the increased adoption of single-use technologies; progress in the medical device field, particularly combinational devices; expanded directives from industry regulators; and advances in analytical technologies.
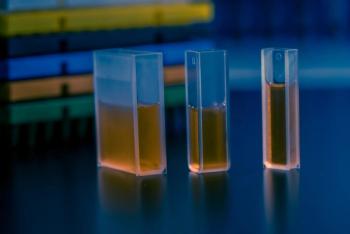
Extractables (1) are defined as compounds that migrate from any product-contact material (including elastomeric, plastic, glass, stainless steel, or coating components) when exposed to an appropriate solvent, under exaggerated conditions of time and temperature. To study materials at risk of potential leachable components, extractions of the contact material are performed, generally using aggressive conditions including acidic, basic, organic, and aqueous solvents. These conditions are not intended to distort the material under investigation but do attempt to mimic the drug formulation. The resulting extracts are usually analyzed using a combination of analytical techniques such as liquid chromatography–mass spectrometry (LC–MS), gas chromatography–mass spectrometry (GC–MS), and inductively coupled plasma–mass spectrometry (ICP–MS) that can qualitatively and quantitatively evaluate both the organic and inorganic components, or “extractables”. Such studies are typically performed to represent a worst-case scenario and may provide an indication of possible leachable components as well as facilitate material selection during early risk assessment.
Leachables (1) are compounds, often identified during extraction studies, that migrate into a drug formulation from any product-contact material (elastomeric, plastic, glass, stainless steel, or coating components). This leaching happens as a result of direct contact under normal process or accelerated storage conditions, such as elevated temperature. However, if the leachable interacts with the drug product (as may be the case particularly with biotherapeutics) or packaging materials, new components can be generated that are known as “secondary leachables”. The complexity of many formulations, often containing a variety of buffers, surfactants, fillers, and other excipients, can lead to the formation of secondary leachables only identified after long-term stability studies.
Biologic E&L studies: the difficulties
E&L evaluation of traditional pharmaceutical medicines is now well established and may be undertaken with a certain predictability in experimental design and even outcome. In contrast, however, certain excipients used in the formulation of some biotherapeutics present unique analytical challenges for leachable determination. Among these excipients are the commonly used nonionic surfactants, such as polysorbate 80 (Tween 80), which constitute a mixture of fatty acid esters of polyoxyethylene sorbitan. These have an extremely low ultraviolet (UV) response but are highly responsive to ionization methods commonly used in LC–MS (2). This often leads to significant interference, either by co-elution and/or suppression during analysis, raising the real possibility of contaminants remaining undetected. Extraction of these surfactants prior to analysis is a possible means of mitigation but is often not highly effective due to the surfactant’s inherent heterogeneity and limited extraction efficiency. Care must also be taken in the application of such an approach since the leachable may be co-extracted with the surfactant.
In the growing area of CGT, there are currently no specific guidelines for E&L studies. However, such products have some unique challenges, such as the use of “ancillary materials”. These materials are used during manufacturing but are not intended to be present in the final product. They are often themselves complex biological materials, such as recombinant insulin and human serum albumin, used as media supplements, and collagen, used as a scaffold in implantable devices (3). Since these materials can potentially interact with and be affected by leachables, in the same manner as the biotherapeutic itself, the choice of materials and controls must be carefully considered to avoid adverse consequences for the manufacturing process.
The evaluation of biotherapeutics for leachables presents many challenges, some of which are somewhat unique to this type of product. For example, the biopharmaceutical itself may interfere in the testing regimen due to its high concentration, heterogeneity, and/or high detector response. A potential solution is to remove the biotherapeutic prior to analysis, but the procedure must be very carefully considered because associated leachables may be unknowingly removed and/or additional extraneous components may be introduced.
The major concern of leachables in pharmaceutical products is their specific toxicity and/or genotoxicity. The additional issue with biotherapeutics is the potential for interaction between the structurally complex biopharmaceutical itself and any leachable components. Compared to traditional pharmaceuticals, proteins and other biotherapeutics are often significantly less stable, due to their strong dependence on physico-chemical and conformational structural properties. These larger molecules often have both hydrophilic and hydrophobic regions, with many reactive sites for possible leachable binding, potentially resulting in the loss of activity via mechanisms such as unfolding, truncation, aggregation, and precipitation. Consequently, the adverse effects of extractables and leachables can be more significant and more difficult to assess on biopharmaceutical products than small molecules. Acrylic acid, for example, a leachable from syringes, has been shown to react at three different sites within a protein structure, resulting in potential changes in charge and hydrophobicity with consequential effects on the therapeutic properties of the protein-based drug (4).
As the manufacture of many biotherapeutics involves cellular-based processes, the presence of certain leachable components can have unfavorable consequences not only on the final drug product but also on the production process itself. Productivity can certainly be adversely affected by leachables that result in cellular toxicity, leading to significant loss in manufacturing yield.
During the past decade, many biotherapeutic manufacturers have migrated to the use of disposable, single-use systems (SUS) for production, and this has now become commonplace in the emerging CGT field. Every operational phase of a biomanufacturing process that uses SUS technology is at risk of leachable contamination. This contamination can be introduced as a result of contact and interaction with different materials, such as polymers, metals, and additives used to construct holding tanks, films, bags, tubing, and filters. This concern extends to containers for buffers, media, water for injection, and other liquids required for manufacturing. The possibility of leachable accumulation may also arise since concentration stages are often used in the manufacturing process.
The majority of biopharmaceuticals are injectable products and, therefore, contaminants enter the bloodstream directly, without the potential for depletion in the gut as with oral medications. In addition, many biotherapeutics, particularly monoclonal antibodies, are dosed in high concentrations (multiple mg/mL) and are produced in liquid, with complex formulations. These drugs can be stored for long periods of time, providing higher risk of leachable adulteration of the product than the solid dose forms common with traditional pharmaceuticals.
Certain products developed in the CGT area can present further challenges for E&L evaluation. Since the quantities of product can be relatively low, the ratio of contact material surface to the drug volume is very high, increasing the potential for leachable contamination. This may be further exacerbated in those treatments that are essentially customized, with each patient receiving the entire product dose.
Product development strategy
Risk assessment in terms of E&L is now an integral part of any product development strategy. This is of particular importance for CGTs, which should not only evaluate the likely compatibility of contact materials used in manufacturing, but also include an experimental study designed to provide an accurate assessment of the extractable and leachable profiles.
While many biotherapeutics are produced as liquid formulations, lyophilized forms of drug product are also commonplace, as part of efforts to improve stability during storage. Interestingly, the FDA Center for Drug Evaluation & Research, the FDA Center for Biologics Evaluation & Research, and the United States Pharmacopeial Convention (in United States Pharmacopeia <1664> [5]), describe sterile powders for injection as being “low risk” for leaching, despite some evidence to the contrary. It has been demonstrated, for example, that several semi-volatile organic compounds originating from butyl rubber stoppers—part of the primary packaging system—may leach into a lyophilized product but not a liquid formulation stored in the same packaging (6). The explanation for this finding lies in the hydrophobicity of the leachables, rendering them very poorly soluble in aqueous media but able to diffuse from the stopper. This is perhaps facilitated by their volatility and the nature of the drug product.
There are multiple types of material used in the manufacture and storage of biopharmaceuticals, and most may be classified as either glass, metal, or synthetic polymer/elastomer. The latter are recognized as the most significant sources of leachables, often resulting from monomers/oligomers of the polymer itself, as well as catalysts, initiators, additives (e.g., lubricants, antioxidants, antitack, and antistatic agents), adhesives, anchoring agents, adhesive resins, colors, fillers, and degradation products of almost all these components. The diversity and nature of these potential contaminants and their often-unpredictable interactions with formulated biopharmaceuticals pose significant challenges to analytical assessment of the drug products and process materials. There are now significant guidance documents available from regulatory authorities, industry organizations, and researchers providing at least some support in the design and rationale for suitable experimental approaches.
For biopharmaceuticals, inorganic leachables (generally associated with glass and metal) are of particular concern because of their potential impact on the stability and efficacy of the drug itself. A metal commonly used is stainless steel, which has found applications in manufacturing, shipping, and storage, and is known to leach iron, chromium, and nickel, particularly if the steel is unpassivated (7). Trace levels of metal ions can potentially cause protein degradation by mechanisms such as protein oxidation and fragmentation. The latter occurs because of the metal-binding propensity of aromatic amino acids such as tryptophan, tyrosine, and histidine. Certain metal–protein binding is also known to induce secondary and tertiary structure changes resulting in the formation of insoluble protein aggregates (8).
Glass has also been demonstrated to be a source of certain metal leachables. For example, manganese and iron oxide—used as coloring agents—are present in Type I amber vials as are zinc and
barium oxides. Higher levels of manganese and iron have been shown to leach from amber glass compared to clear glass. Meanwhile, sterilization techniques, such as steam autoclaving and gamma irradiation, may also lead to the presence of metal ion contamination (9).
Some biotherapeutic excipients, and the drug itself, may also play a significant role in facilitating the extraction of metals from contact surfaces. Certain proteins and chelating agents, such as ethylenediaminetetraacetic acid, have been shown to increase the quantity of metals such as aluminum, calcium, and iron from plastic container systems. Similarly, buffers such as phosphate and lactate can also increase the metal leaching from both metal and glass surfaces.
The area of E&L investigation has developed rapidly over the past decade, resulting in technological and regulatory advancement. Ultimately, this has led to safer medications. However, developments in biopharmaceuticals and specifically in CGT are likely to present further demands on expertise in areas of manufacturing and analytics.
It is clear that a single, common strategy, for monitoring and/or eliminating leachable contaminants will never be sufficient to address all situations. Instead, engineers and investigators must be always prepared for the unexpected.
References
1. D.B. Lewis, “Current FDA Perspective on Leachable Impurities in Parenteral and Ophthalmic Drug Products,” Presentation at AAPS Workshop on Pharmaceutical Stability—Scientific and Regulatory Considerations for Global Drug Development and Commercialization (Washington, DC, Oct. 22–23, 2011).
2. J. Fukuda, et al., J. Chromatogr. B 953–954, pp. 68–72 (2014).
3. J. Solomon, et al., Cytotherapy 18 (1) 1–12 (2016).
4. D. Liu, et al., PDA J Pharm Sci Technol. 66 (1) 12–19 (2012).
5. USP, USP General Chapter <1644>, “Assessment of Drug Product Leachables Associated with Pharmaceutical Packaging/Delivery Systems,” USP 38-NF 33, first supplement (Rockville, MD, Aug. 1, 2015).
6. S.A. Zdravkovic, J. Pharm. Sci. 107 (11) 2837–2846 (2018).
7. L. Allain and Q. Wang, Am. Pharm. Rev. 10 (3) (2007).
8. J.L. Cleland, M.F. Powell, and S.J. Shire, Crit Rev Ther Drug Carrier Syst 10 (4) 307–77 (1993).
9. D. Bohrer, et al., J Trace Elem Med Biol 17 (2) 107–115 (2003).
About the author
Mark Rogers, PhD, mark.rogers@sgs.com, is the global scientific director for the SGS Health Science Drug Development group.
Articles in this issue
over 4 years ago
Thermo Fisher Expands Hematology Oncology NGS Portfolioover 4 years ago
Summa Equity Acquires Majority Stake in Axion BioSystemsover 4 years ago
Artificial Intelligence Facilitates Empty Well Detectionover 4 years ago
J.T.Baker Robotic Tips from Avantor Offer Precision WorkflowNewsletter
Get the essential updates shaping the future of pharma manufacturing and compliance—subscribe today to Pharmaceutical Technology and never miss a breakthrough.